Transcranial magnetic stimulation (TMS) offers hope for patients with treatment-resistant depression. As one doctor at the University of California in San Diego reveals, the technology could be game-changing for individuals suffering from chronic mental illness.
Major depressive disorder is the leading cause of disability in the U.S. for ages 15 to 44. The disease affects more than 16 million American adults, or approximately 6.7 percent of the U.S. population age 18 and older in any given year, according to the National Institute of Mental Health.
Depression is frequently treated with psychotherapy or pharmaceutically with selective serotonin reuptake inhibitors (SSRI), dopamine-norepinephrine reuptake inhibitors, or serotonin-norepinephrine reuptake inhibitors. Unfortunately, these approaches have been found to be ineffective for nearly one-third of patients. This leaves clinicians and researchers always on the lookout for promising new depression treatments.
TMS — also called rTMS for repetitive transcranial magnetic stimulation — clinical trials have shown a 50 percent reduction in symptoms for about half of patients with treatment-resistant depression. A third of patients achieved complete remission following the trial.
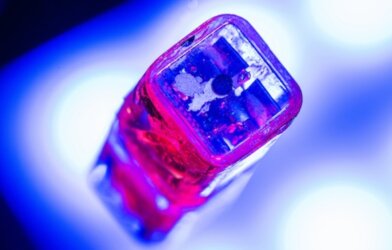
The prototype for TMS was developed in the 1980s. A decade later, small-scale studies began. By the 2000s, there was a pivotal trial that led the Food and Drug Administration to approve TMS in 2008 for treating antidepressant-resistant depression. Currently, it’s also approved for smoking cessation and obsessive-compulsive disorder.
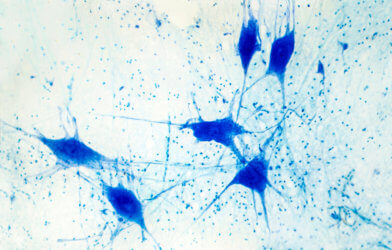
The TMS device itself contains a coil of wires that emit a magnetic pulse. This generates a tiny electrical field inside the brain that excites neurons near the surface. There are few reported side effects and the process is pain-free for the overwhelming majority of patients, who liken it to a fingernail tapping on the forehead.
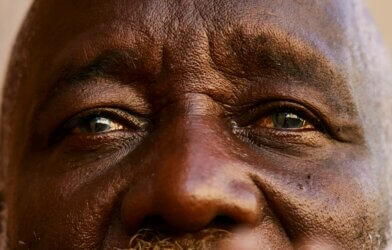
Teresa Lindhart is just one of the many patients who has seen results from TMS. After six weeks of daily treatments with TMS, Lindhardt, 55, says she’s completely free of the symptoms of depression that disrupted, and twice nearly ended, her life. Lindhardt has been on SSRIs, but they were not enough to control suicidal ideation. She also found that the side effects of the SSRIs required further medication to keep under control. “For me, this has been the most life-changing thing that has ever happened,” said the former X-ray technician, who first noticed the difference two weeks into treatment. “I look forward to things. I’m not exhausted. I have my life back.”
“The idea that you can transform a person’s life like we did with Teresa with a relatively brief, easy-to-use and very well-tolerated treatment is quite heartening,” said Zafiris “Jeff” Daskalkis, MD, PhD, chair of the Department of Psychiatry at UC San Diego School of Medicine.
It remains unlikely that TMS will become a frontline treatment for depression, replacing medications. “It may very well be an exceptional idea to upstream TMS earlier in the course of treatment,” Daskalakis said. “But we don’t know if it is in any way superior or equal in efficacy to medications. And, the truth is, it’s not going to scale as effectively as medications are. You can access a whole lot more people with medications than you can with TMS.”
This report was published by UCSanDiego.
Article by Rhonda Errabelli