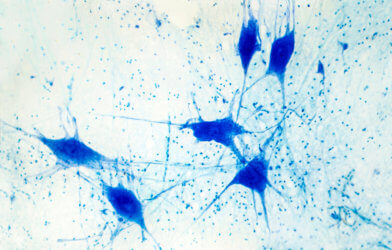
The development of cognitive symptoms in those who have been infected with a mild case of COVID appears to coincide with abnormalities in the cerebrospinal fluid. Researchers believe the preliminary findings could help scientists better understand how the SARS-CoV-2 virus affects the brain. That’s especially the case at least in those patients who experienced a mild COVID infection that did not require hospitalization.
Researchers from the University of California, San Francisco, and Weill Cornell Medicine in New York analyzed the cerebrospinal fluid of 17 volunteers who had previously been infected with COVID. Thirteen of these participants had experienced “brain fog” post-COVID, which means the impairment of certain executive cognitive functions, such as focus, memory, and processing speed.
Lumbar punctures were performed on participants ten months after their initial COVID symptom on average. No abnormalities were found in the four participants who exhibited no cognitive symptoms post-COVID.
But of the 13 participants who had exhibited post-COVID cognitive symptoms, 10 had noticeable abnormalities in their cerebrospinal fluid. These irregularities included the presence of unexpected antibodies and elevated levels of protein.
Some antibody abnormalities were limited to the cerebrospinal fluid, indicating inflammation solely of the brain, while others were detected in both cerebrospinal fluid and blood. The source and cause of these unexpected antibodies were uncertain and could be so-called “turncoat” antibodies, which actively attack the body rather than a foreign antigen.
“It’s possible that the immune system, stimulated by the virus, may be functioning in an unintended pathological way. This would be the case even though the individuals did not have the virus in their bodies,” said senior author Joanna Hellmuth in a statement.
The detected abnormalities are similar to those found in patients with other infectious diseases and may provide key insights into why some patients develop so-called “brain fog’ after a mild bout with COVID, while others do not. Other viruses that have been known to cause cognitive symptoms include HIV, Epstein-Barr, and hepatitis C.
Additionally, the presence of underlying risk factors for cognitive impairment, such as hypertension, ADHD, and anxiety, appears to increase the likelihood of a patient developing cognitive symptoms post-COVID. Those participants who developed cognitive symptoms had an average of 2.5 cognitive risk-factors pre-infection, while those without symptoms had less than one risk factor.
Age may be an additional risk factor to consider, as the average age for participants with cognitive symptoms was 48, compared to 39 for those without symptoms.
The small scale of this study may limit the scope of its findings, but researchers are optimistic that this initial data could lead to a greater understanding of how COVID impacts both the brain and immune system. This new information could improve both the diagnostic approach towards those afflicted with cognitive symptoms post-COVID and eventually lead to a new line of treatments, as well.
This study is published in the Annals of Clinical and Translational Neurology.
Article written by Adam Swierk