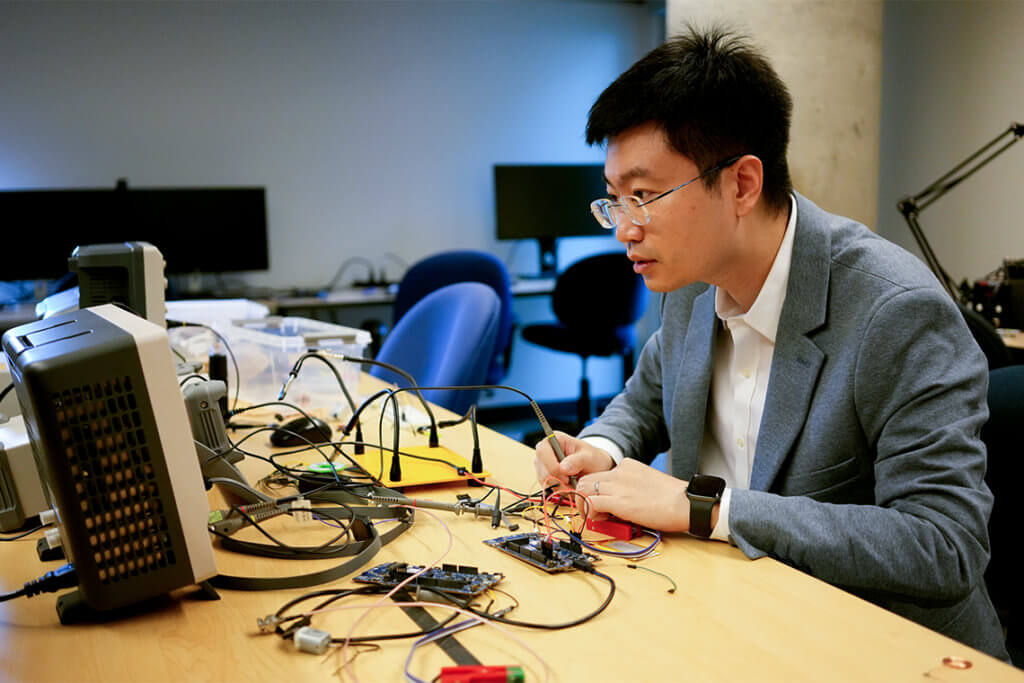
At the University of Toronto, Dr. Xilin Liu is creating smarter, safer, neural implants with microelectronics and artificial intelligence (AI) to treat brain disorders such as Parkinson’s disease and epilepsy.
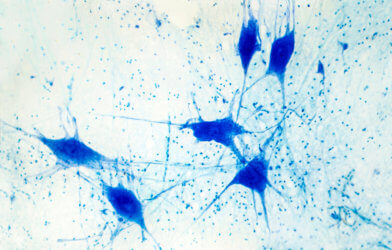
“Neurons talk to each other in part via electrical signals, and a therapeutic neural implant produces electrical stimulation – like a pacemaker for the brain,” says Liu, in a statement. An assistant professor in the Faculty of Applied Science & Engineering, Liu explains, “In cases of tremors or seizures, the stimulation attempts to restore the neurons to a normal condition. It’s as if the stimulus turns the neural networks off and on – almost like restarting a computer, though it’s definitely not that simple. Scientists don’t fully understand how it works yet.”
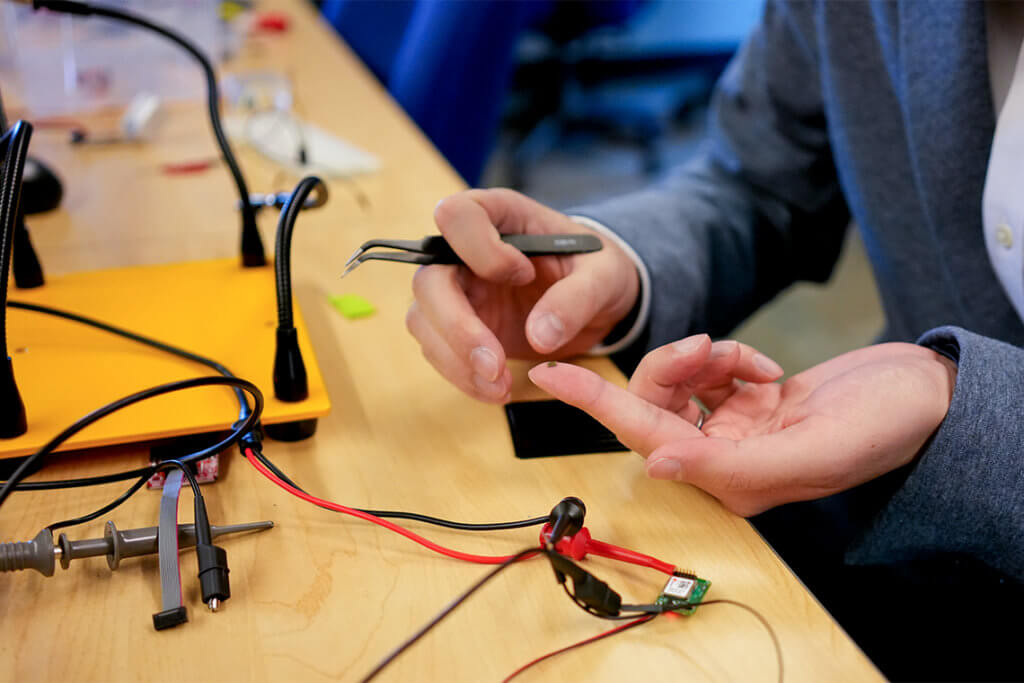
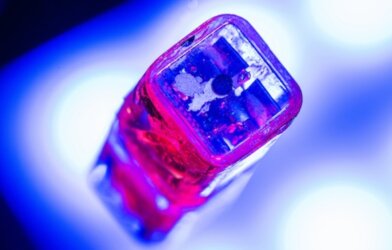
The neural implants consist of miniature silicon chips, manufactured using the same process used for fabricating chips used in PCs and smartphones. The new technology, referred to as a complementary metal-oxide semiconductor (CMOS), makes for reduction of the device’s size and power consumption, lessening the risks associated with surgical implantation and long-term use.
“We’ve developed many new microelectronic design techniques, such as high precision electrical stimulation with charge balancing,” says Liu. “We try to come at the problem from many different angles.”
In a recent project, Liu and his team used the power of AI as “deep learning” (DL) to maximize the implants’ efficacy and minimize excessive stimulation.
“Most existing implants produce electrical stimulation at a constant rate, regardless of the patient’s condition,” says Liu. “With DL, we can activate the neural implants at the optimal time and only when necessary.”
There is a high computational cost for the technology, leading the research team develop techniques for training and optimizing the models for individual patients’ conditions.
According to Liu, the technology has a broad range of clinical applications usable for many of the one billion people worldwide suffer from various brain disorders.
Liu wants to impress on the graduate students whom he teaches that collaboration is essential to advancing the neural implant field. “There’s so much going on in the brain,” he says. “You need a range of experts to understand and provide solutions for these disorders, which will only become more common as human life expectancy increases.”
Future conditions for exploring the effectiveness of the neural implants include chronic pain, depression, and dementias.
This work is published in the Journal of Neural Engineering.