A teacher diagnosed with narcolepsy says the “date rape drug” GHB has transformed her life and helped her to live with the incurable condition.
Heather McFarlane, 47, from Glasgow, Scotland suffers from cataplexy and narcolepsy. When she laughs, she loses control of her muscles, and falls asleep uncontrollably. She began to experience symptoms after having her third child in 2010. The sleep disorder meant she had to give up driving.
McFarlane, who worked as a teacher for kids with additional needs, avoided watching comedy shows on TV after a routine by British comedian Peter Kay triggered the initial onset of the illness. Three years later she got a diagnosis, after falling asleep in the middle of conversations.
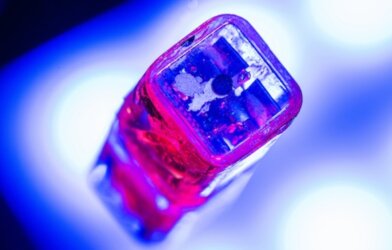
She now takes the medication sodium oxybate, a purified form of GHB, which allows her to live a “normal” life. The drug helps her to sleep at night and stay awake during the day. GHB is well known as the “date rape drug,” but has been used clinically to treat narcolepsy for several years.
“I was laughing and within a split second it looked like I was asleep, but I was lying there and I couldn’t move any muscles,” McFarlane tells South West News Service. “It was horrible. I was still awake and conscious, but I was essentially trapped in my body.”
The new mom found she was struggling to stay awake and that emotions, such as laughter or smiling, could trigger an attack — where her face muscles would droop and her legs would give way.
At work at Hazlewood School in Glasgow, Scotland, McFarlane would retreat to the staff restroom where she would end up asleep. She had to give up driving the school bus.
“It was horrendous,” she recalls. “When I laughed, I had a kind of shutdown, as if I had rebooted in a split second – like the power had gone out and come back on again. I had to stop watching funny things on TV and avoiding funny situations with the kids. It saw part of me disappear. I even had to learn to function as a different kind of mum to the one that I was.”
McFarlane sought help from her doctor and in 2013, was referred to a specialist team at Glasgow Royal Infirmary for support, where she was finally diagnosed.
“It was a game-changer in lots of different ways. I’ve been able to get some of my life back,” she says. “The team have been amazing. It’s not just the condition they are interested in, it’s me as a person – and not just me, but my wider family as they know this impacts all of us. It’s hard to live in Glasgow and have to avoid things which are funny – now I don’t have to.”
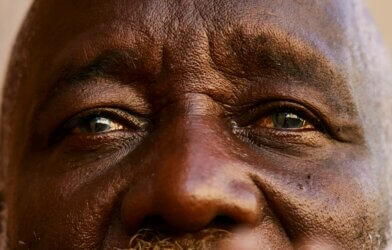
Dr. Eric Livingston is a respiratory consultant and clinical lead at the clinic. “When we get the medication right, it can transform lives, allowing people to drive their cars again, or get back to work or university – instead of people thinking they are tired or lazy,” he says. “Some people have been told for 30 years that they are lazy, before they even get a diagnosis, but we can support and get them back to a full life again.”
Article by South West News Service writer Sarah Ward