When you hear the word “stroke,” what are your first thoughts? For a lot of people, those thoughts are of paralysis of some part of the body, a loss of function, language disorders and the unknown – can that function lost be restored? Scientists at Hiroshima University (HU) have started human trials for a new stem cell treatment that shows promise of answers for some unknowns – even potentially reversing paralysis and language disorders after moderate to severe strokes.
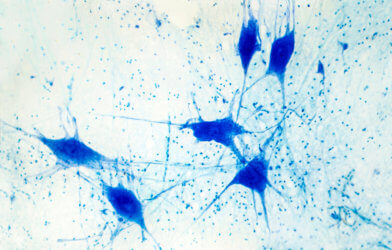
They are using mesenchymal stem cells (MSCs) derived from cranial bone. This unprecedented clinical trial is the work of Department of Neurosurgery Professor Nobutaka Horie and Assistant Professor Takafumi Mitsuhara, along with Bio-Environment Adaptation Sciences Professor Rui Yugeand.
Previously, the Japanese team demonstrated that cranial bone derived MSCs led to return of some function in rat models of stroke and spinal cord injury.
The therapy uses autologous MSCs from the patients’ own cranial bones to treat for moderate to severe cerebral infarctions. With currently available treatments, restoration of neurological recovery is extremely difficult or impossible. These devastating strokes occur when blood and oxygen supply to the brain are disrupted, usually by a blood clot blocking blood flow to the brain.
A stroke can cause a rise in intracranial pressure that contributes to lasting brain injury or death. In these patients, neurosurgeons often perform extracranial decompression. A large segment of the skull is removed, and the dura mater, a thick membrane made of dense, irregular connective tissue that surrounds the brain and spinalcord, is replaced with a substitute, such as artificial dura mater.
Even if the surgery saves lives, it cannot reverse the damage inflicted on the brain. Many patients, after moderate to severe stroke, suffer severe residual disabilities and need help for basic self-care for the rest of their lives. Some of these residual deficits include paralysis, language deficits, cognitive decline, dysphagia or difficulty in swallowing, spasticity or muscle stiffness, depression, and urinary disorders.
A 2007 survey administered by Japan’s Ministry of Health, Labour and Welfare showed that stroke is Japan’s second most common cause of dementia and the leading reason for becoming bedridden. According to the researchers, stroke cases in Japan are expected to more than double from 1.3 million in 2019 to three million in 2025 as the population ages.
MSCs are both multipotent and can become specific types of cells. Their characteristics may vary depending on the tissue of origin. The researchers said that cranial bone derived MSCs are superior to the ones isolated from the iliac bone, which is the most common source of MSCs. The cranial MSCs can differentiate into nerves. A previous study using rats showed, also, that MSCs from rat and human cranial bones have many neurotrophic factors, proteins that strengthen neuron health and functional recovery. The target number of patients for the clinical trial is six.