A so-called “brain switch” behind memory loss has been identified by scientists. Turning it back on could combat Alzheimer’s disease and other age related neurological disorders, new research shows.
The system lies in the hippocampus – the memory control center of the brain. Its discovery sheds fresh light on the causes of dementia.
“We are trying to understand normal memory and why a part of the brain called the hippocampus is so critical for normal memory,” says study senior author James Knierim, a professor at Johns Hopkins University’s Zanvyl Krieger Mind/Brain Institute, in a statement. “But also with many memory disorders, something is going wrong with this area.”
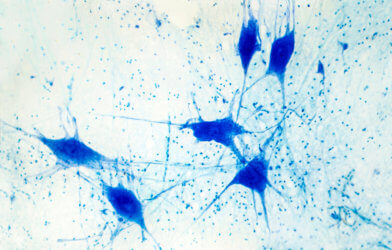
The mechanism lies in a tiny region named CA3. It lies deep in the brain’s temporal lobe, within the hippocampus. It helps us recognize patterns, influencing the fine balance between pattern separation and completion operations, and, consequently, learning and memory.
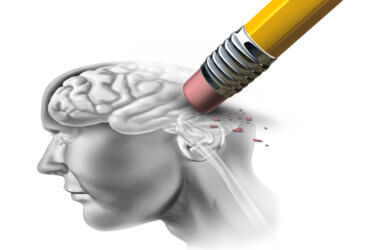
When they swing out of balance, memory becomes impaired, causing symptoms like forgetfulness or repeating oneself. The scientists discovered that as the brain ages, this imbalance may be caused by the loss of CA3. The pattern separation function fades away, and the pattern completion function takes over.
Neurons responsible for each are typically more prevalent in the center and at the edge, respectively. With aging, activity in the middle becomes overactive, and the interplay between the two regions becomes abnormal, creating a dominance in pattern completion.
In normal brains, pattern separation and pattern completion work hand-in-hand to sort and make sense of perceptions and experiences, from the most basic to the highly complex. If you visit a restaurant with your family and a month later you visit the same restaurant with friends, you should be able to recognize it was the same restaurant, even though some details have changed. This is pattern completion.
But you also need to remember which conversation happened when, so you do not confuse the two experiences. This is pattern separation.
When pattern separation disappears, pattern completion overpowers the process.
With your brain focusing on the common experience of the restaurant to the exclusion of the details of the separate visits, you might remember a conversation about a trip to Italy during one visit, but mistake who was talking. “We all make these mistakes, but they just tend to get worse with aging,” says Kneirim.
In experiments, the researchers compared young rats with unimpaired memories to older rats with unimpaired or impaired memories. The older rats with unimpaired memories performed water maze tasks as well as young rats.
But neurons in the CA3 region were already beginning to favor pattern completion at the expense separation. The physiological finding had not shown up in their behavior. Something was allowing the rats to compensate for the deficit. It is echoed in humans who remain surprisingly sharp into their older years.
Pinpointing the memory loss mechanism could lay the groundwork for learning what prevents impairment in some people – opening the door to preventing or delaying cognitive decline in the elderly.
“If we can understand better what these compensatory mechanisms are, then maybe we can help prevent cognitive decline with aging,” says Knierim. “Or, if we can’t stop it, maybe we can enhance other parts of the brain to compensate for the losses that are occurring.”
The same team previously demonstrated the anti-epilepsy drug Levetiracetam improves memory performance by reducing hyperactivity in the hippocampus. The latest, more specific information about how memory impairment occurs might allow scientists to better aim such drugs toward the deficits in the future.
“It would give us better control of where we could possibly target the deficits that we see,” explains lead author Heekyung Lee, an assistant research scientist in the lab.
The number of people worldwide with Alzheimer’s disease and other forms of dementia is predicted to triple by 2050 because of aging populations. Current drugs can only treat the symptoms – not the cause.
The study is published in the journal Current Biology.
Report by Mark Waghorn, South West News Service