Lou Gehrig, (aka the Iron Horse), was dubbed the “greatest hitter of all time” during his 17 seasons with the New York Yankees. His world, and the world of baseball, was of course famously turned upside down upon his diagnosis of amyotrophic lateral sclerosis (ALS) at age 36. He said at the time: “I thought of my new uncertainty: How long can I live with ALS? I thought: ‘Don’t search for answers. Live the question.’ Enjoy life more because of the uncertainty, not less.”
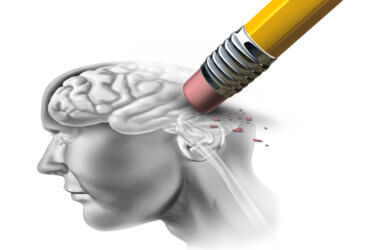
ALS (also called Lou Gehrig’s disease) is a progressive disease that affects nerve cells in the brain and spinal cord, causing loss of muscle control. There is no cure. One third of patients die within one year of diagnosis. Scientists at the National Institutes of Health (NIH), in collaboration with scientists at University College London (UCL) have revealed, for the first time, why a common genetic variant worsens disease outcomes for people with the devastating adult-onset ALS and another neurodegenerative disease called frontotemporal dementia (FTD).
Frontotemporal dementia is a related disease with similar underlying causes. Symptoms include language impairment, changes in personality, and cognitive difficulties.
The study shows that depletion of the TDP-43 protein is associated with 97 percent of ALS cases and 50 percent of FTD cases. The depletion corrupts the genetic instructions for the critical neuronal UNC13A protein. UNC13A enables neuron-to-neuron communication by the release of neurotransmitters. Its loss can be fatal.
Researchers say that a genetic variant, previously associated with disease risk, increases the chance of UNC13A’s genetic instructions being corrupted among people with the diseases. The variant increases the risk and severity of ALS and FTD. The discovery raises hope for new treatments. By developing a therapy that blocks the corruption of UNC13A’s genetic instructions, disease progression could be slowed for most people with ALS and about half of patients with FTD.
“The majority of research into gene therapy has focused on genes implicated in familial ALS (patients with a family history of the disease), but the vast majority of ALS cases are sporadic, with no known family history,” says professor Pietro Fratta, from the UCL Queen Square Institute of Neurology, in a statement.
Adds Dr. Michael Ward, of the National Institute of Neurological Disorders and Stroke: “We have known for a long time that genetic variants in UNC13A cause an increased risk of ALS and dementia, but nobody had figured out why this is the case. Together, our teams showed exactly how this genetic risk factor for ALS interplays with the core disease mechanism, TDP-43 loss, in order to worsen the disease course.”
The most important protein in ALS research is TDP-43; in most cases the protein is incorrectly ejected from the cell’s nucleus. This prevents TDP-43 from performing its vital functions, such as ensuring that mRNA is replicated correctly.
“We have known for a long time that most patients with ALS, and about half of FTD patients, lose the function of a key protein called TDP-43, wreaking havoc in nerve cells that are affected,” says Dr. Ward. “But we haven’t known how to reverse the most problematic consequences of TDP-43 loss.”
As part of the experimental study, the researchers used human stem cells to make neuronal cells in dishes and removed the TDP-43 protein from these cells using a Nobel prize-winning gene-editing technology – CRISPR-Cas9.
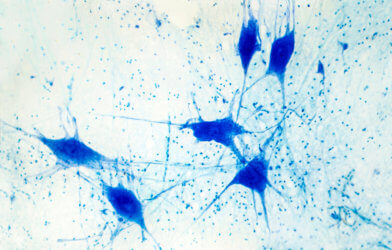
The scientists studied how these neurons without TDP-43 differed from normal neurons. They found that the mRNAs for the UNC13A protein were corrupted, meaning that the lab-grown neurons were unable to correctly produce the UNC13A protein. Furthermore, when the team looked at ALS and FTD patient brain samples, they again found that the mRNAs for UNC13A were incorrect, confirming that their experiments accurately replicated the in-vivo process.
Given the essential role UNC13A plays in facilitating neuron communication, its corruption will impair neuronal function, contributing to neurodegeneration in patients with ALS and FTD.
“We have built on years of genetic research that identified that UNC13A was implicated in motor neuron disease and FTD, and supported it with a new molecular biology finding that confirms that the gene is absolutely fundamental to the disease process,” says Fratta. “We are hoping to carry out trials over the coming years to develop such a treatment that could potentially greatly improve the lives of people living with ALS.”
The findings are published in the journal Nature.